Oral Presentation Australian Diabetes Society and the Australian Diabetes Educators Association Annual Scientific Meeting 2014
Impact of Specialised Inpatient Diabetes Service on Hospital Stay and Complications (#55)
BACKGROUND
Up to 30% of hospital inpatients have been reported to have diabetes. Hyperglycaemia is associated with increased morbidity and mortality (1,2). Although protocol-driven intensive glucose targets in critical care settings have not been consistently justified, improved glycaemic regimens with less stringent glycaemic targets in non-critical care surgical inpatients may be associated with reduced hospital complications (3).
METHODS
A specialised inpatient diabetes management service (IDMS) was established at Westmead Hospital in 2012. Retrospective review of health outcomes in surgical inpatients prior to and after establishment of the service were analysed by:
(i) Average length of stay (LOS) in inpatients with diabetes, identified by Diagnoses Related Group (DRG) codes, compared against national health round table (HRT) benchmarks, prior to and after IDMS commencement.
(ii) Medical record review of glycaemic outcomes, LOS and a composite outcome of sepsis, acute renal failure, cardiac events and HDU/ICU stay in a cohort of 69 consecutive patients with diabetes over a month in 2012, was compared to patients with diabetes, identified via DRG, in the same month (n=54) of the preceding year.
RESULTS
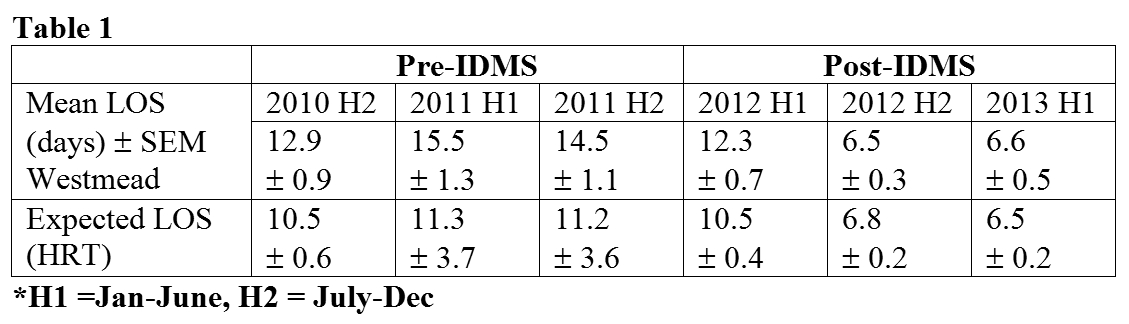
Average LOS of inpatients with diabetes at Westmead Hospital, identified by DRG codes, exceeded expected LOS in the half years from 2010-2011; but after the introduction of the service in 2012, progressively fell to that of expected LOS.
In the sub-cohorts with detailed record review, the composite of adverse health outcomes , after introduction of the service, was reduced relative to that in the previous year. (2011=51.9%; 2012=24.3%, p=0.002). Logistic regression analysis indicated a statistically significant impact on the composite after adjusting for expected LOS (OR 0.352 [95% CI 0.158-0.784], p=0.0011)
CONCLUSIONS
The introduction of a specialised inpatient diabetes service may result in reduced complications and length of stays in surgical inpatients with diabetes.
- Underwood P, Askari R, Hurwitz S, Chamarthi B, Garg R. Preoperative A1C and clinical outcomes in patients with diabetes undergoing major noncardiac surgical procedures. Diabetes Care 2014; 37: 611-6
- Cheung NW, Wong VW, McLean M. The Hyperglycemia: Intensive Insulin Infusion in Infarction (HI-5) study: a randomized controlled trial of insulin infusion therapy for myocardial infarction. Diabetes Care 2006; 29: 765-70
- Umpierrez, GE et al Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes undergoing general surgery (RABBIT 2 surgery). Diabetes Care 2011, 34(2), 256-261