Oral Presentation Australian Diabetes Society and the Australian Diabetes Educators Association Annual Scientific Meeting 2014
Sitagliptin is more effective than Gliclazide in Preventing Pro-Fibrotic and Pro-Inflammatory Gene Expression Changes in a Rodent model of Diet-Induced Non-Alcoholic Fatty Liver Disease (NAFLD) (#84)
This study of NAFLD induced by high fat diet causing obesity examined whether sitagliptin and gliclazide have similar protective effects on pathological liver changes and potential mechanisms for the in vivo observations.
Methods: Wild type C57BL/6 male mice were fed ad libitum a high fat diet (HFD) or standard chow (CHOW) for 15 weeks. Following randomization, in some mice equipotency oral sitagliptin or gliclazide were provided in food for the final 10 weeks before termination. Livers were frozen for mRNA measures by qPCR and second messenger ERK protein was examined by Western immunoblot. Subsequently, primary hepatocytes were isolated and treated with the saturated fatty acid palmitate(200μM), with or without equimolar sitagliptin or gliclazide, and mRNA was then measured by qRT-PCR at 24h and 48h.
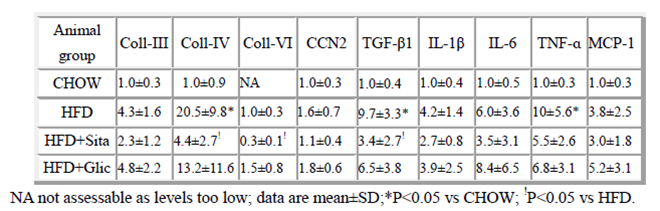
Results: Mice were on average 31% heavier in the HFD than in CHOW (each P<0.05), but were non-diabetic. Sitagliptin prevented pro-fibrotic marker induction of pathological collagen-IV,-VI, and TGF-β1 each more effectively than gliclazide, and showed trends collagen-III and CCN2 regulation (Table).Pro-inflammatory gene induction of IL-1β, IL-6, TNF-α, and MCP-1 mRNA each showed a non-significant trend to greater normalisation with sitagliptin than gliclazide (Table). Sitagliptin had greater ability than gliclazide to normalise total ERK dysregulation in whole liver measured by Western immunoblot. Autophagy protein markers induced by HFD in liver (LC-3 and Beclin-1) were also inhibited by sitagliptin more than gliclazide (not shown). Consistent with the in vivo data, in cultured hepatocytes, sitagliptin (200μM) inhibited certain pro-fibrotic (col-III, fibronectin, CCN2, TIMP-1 and TGF-β1, each P<0.05) gene expression induced by palmitate, while gliclazide had no effect.
 Conclusion:
This data indicates that sitagliptin compared
with gliclazide, exhibits greater inhibition of pro-fibrotic and pro-inflammatory
gene induction in a HFD NAFLD model. The data suggests that sitagliptin therapy
may have specific benefit in diet-induced NAFLD.
Conclusion:
This data indicates that sitagliptin compared
with gliclazide, exhibits greater inhibition of pro-fibrotic and pro-inflammatory
gene induction in a HFD NAFLD model. The data suggests that sitagliptin therapy
may have specific benefit in diet-induced NAFLD.