Poster Presentation Australian Diabetes Society and the Australian Diabetes Educators Association Annual Scientific Meeting 2014
Professional (Retrospective) Continuous Glucose Monitoring: a retrospective analysis of its use in an outpatient clinic setting (#338)
Background
Self-monitored blood glucose levels (SMBG) to guide changes to therapy is routinely practiced but is inherently problematic. Continuous glucose monitoring (CGM) delivers a glucose result every 5 minutes. Professional CGM is a form of monitoring where the patient is unaware of the result during the period of monitoring, typically 3-7 days. There is conflicting evidence regarding the impact of professional CGM on lowering of elevated HbA1c levels and reduction in frequency and duration of hypoglycaemia.1-3 Given conflicting data and lack of a universally accepted clinical practice protocol, we analysed the use of professional CGM in the real-life outpatient setting.
Subjects and Methods
We reviewed 113 consecutive patients undergoing professional CGM between 2009-2014 at RMH (Table below) using the iPRO device (Medtronic).
Results
Mean time to follow-up with a health professional following CGM was 63 days (range 6-368 days). In 32 (29%) patients there was no documented change to management after CGM. For these patients, the mean time to follow-up was 100 days compared to 48 days for patients with one or more documented change to management (p<0.005). Comparison of HbA1c before CGM and 3-9 months after the follow-up appointment demonstrated a reduction of 0.35% in those patients with an initial HbA1c >8% compared to a rise of 0.34% in those with initial HbA1c <8% (p<0.001). For patients with at least one documented change to management, the drop in HbA1c in those with an initial HbA1c >8% was more pronounced (-0.42%).
Conclusion
Our findings suggest that professional CGM may have a beneficial role in improving glycaemia, particularly where treatment recommendations are made/documented. Treatment recommendations were more likely when review occurred closer to the time of CGM. Our findings highlight the need for systematic follow-up and intervention following professional CGM to optimise its utility in the outpatient setting.
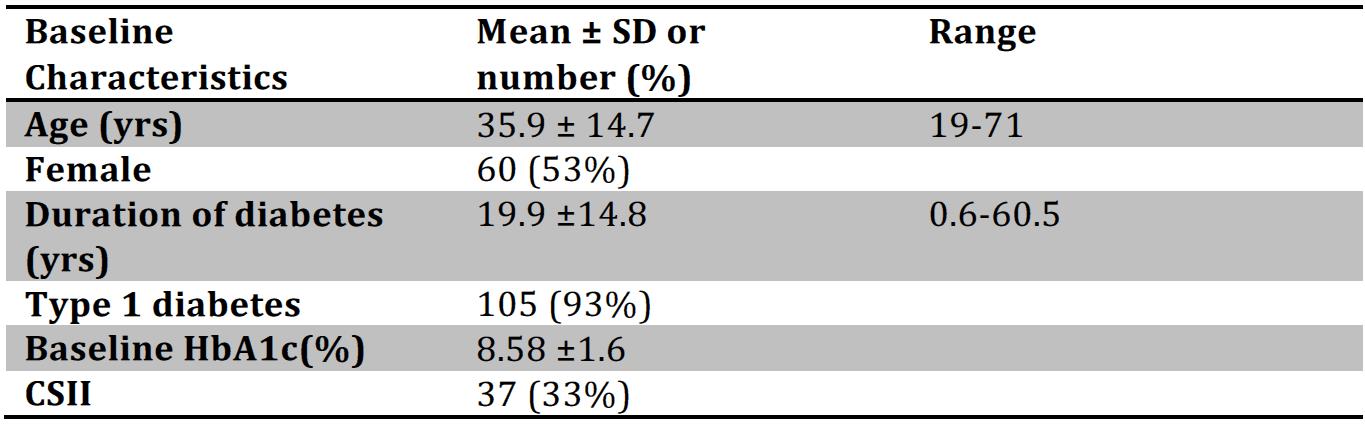
CSII = continuous subcutaneous insulin infusion
- Leinung M et al. Benefits of short-term professional continuous glucose monitoring in clinical practice. Diabetes Technology & Therapeutics 2013; 15: 744-747
- Miele A et al. Clinical outcomes associated with referral-based continuous glucose monitoring using a central standardised interpretation strategy. Diabetes technology & therapeutics. 2012; 14: 765-771
- Pepper GM et al. Effect of short term iPro continuous glucose monitoring on haemoglobin A1c levels in clinical practice. Diabetes technology & therapeutics. 2012; 14: 1-4