Poster Presentation Australian Diabetes Society and the Australian Diabetes Educators Association Annual Scientific Meeting 2014
Complication differences in early versus late diagnosis of autoimmune diabetes in adults (#290)
Background & Aim
Although complication prevalence has been reported in latent autoimmune diabetes in adults (LADA) most studies have focussed on comparisons with type 1 and type 2 diabetes. We aimed to determine if earlier versus later diagnosis of islet autoimmunity, in relation to diabetes diagnosis, was associated with differences in diabetes complication prevalence and glycaemia.
Methods
The study was a retrospective clinical audit of 109 cases of LADA (age>25y, islet autoantibody positive, non insulin requiring for 36 months post diagnosis of diabetes) followed for a minimum of 5 years and a maximum of 15 years. Data were obtained from hospital records, diabetes databases and patient questionnaires. The LADA cohort was divided in to two groups, early and late diagnosis, based on the median time to recognition of islet autoimmunity positivity after diabetes diagnosis (0.9y).
Results
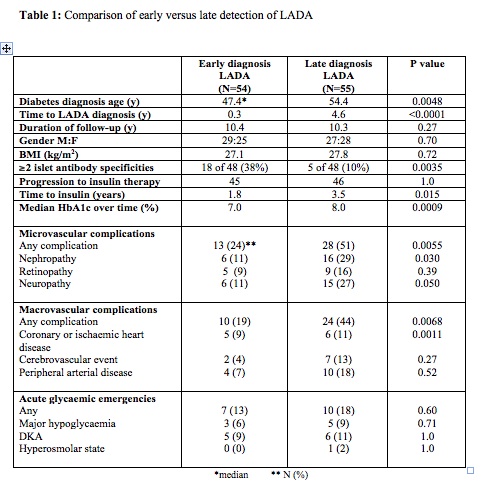
The median time to diagnosis in the early diagnosis LADA group was 0.3 years compared to 4.6 years in the late diagnosis group. The median follow-up time for both groups was 10 years (Table 1). The late diagnosis group progressed to insulin significantly later at 3.5 years post diagnosis of diabetes and had a significantly higher HbA1c over time (late diagnosis 8.0 vs 7.0%, P=0.0009) (Table 1). The late diagnosis group had more nephropathy (51% vs 24%, p=0.0055) and ischaemic heart disease (44% vs 19%, p=0.0068) complications (Table 1).
Conclusion
This study suggests diabetes-related complications may be more prevalent in later diagnosis of autoimmune diabetes in adults. Larger studies integrating primary, secondary and tertiary care data are required to investigate these observations and exclude ascertainment biases.