Oral Presentation Australian Diabetes Society and the Australian Diabetes Educators Association Annual Scientific Meeting 2014
SUICIDAL IDEATION AND SELF-HARM IN TYPE 1 AND TYPE 2 DIABETES: RESULTS FROM DIABETES MILES - AUSTRALIA (#51)
Background: Depressive symptoms are common among people with diabetes, and may be accompanied by suicidal ideation (SI). We aimed to explore the prevalence of SI amongst adults with diabetes, and determine correlates of SI, independent of depression. We utilised data from the Diabetes MILES-Australia study, a comprehensive national survey of adults with type 1 or 2 diabetes, focused on the psychosocial and behavioural aspects of living with diabetes.
Methods: A random sample of 15,000 National Diabetes Services Scheme registrants were mailed a survey booklet, with an online version of the survey advertised nationally. Participants (N=3,338) completed validated self-report measures as well as study-specific items. Data extracted for the current analyses included those relating to depression (PHQ-9; including item 9 concerning SI and self-harm), diabetes-specific distress (PAID), social support, and clinical and demographic details. Controlling for depression, a separate logistic regression analysis was conducted for each dependent variable to explore the relationship with SI.
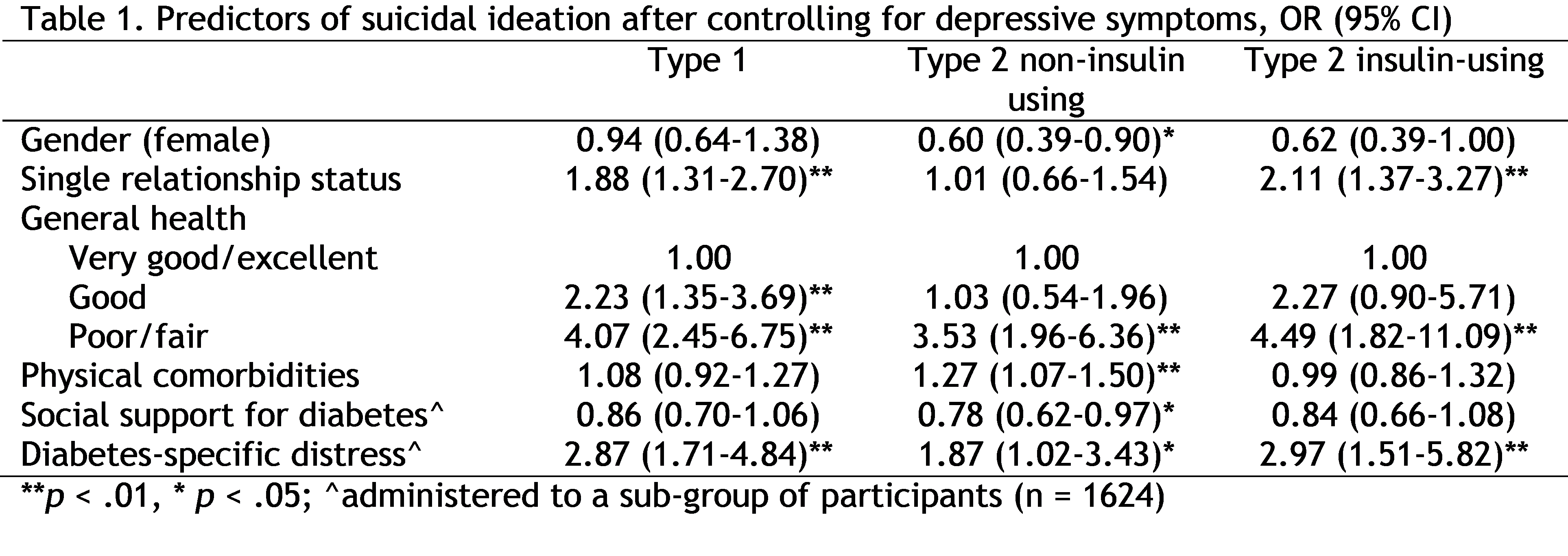
Results: In total, 14% (N=472) reported SI or self-harm: 14% (N=189) of adults with type 1 diabetes, 12% (N=148) with type 2 diabetes not using insulin (N=135), and 19% with type 2 diabetes using insulin. SI was significantly more common among adults with elevated levels of depressive symptoms (40.6%) than those without (5.8%). After controlling for depression, SI was predicted by the factors showing significance in Table 1.
Conclusions: For those using insulin, suboptimal health, elevated diabetes-specific distress and being single were strong predictors of SI. For those with type 2 diabetes not using insulin, predictors were broader, reflecting poor health and comorbidities. These findings suggest the importance of integrating physical and mental health care for people with diabetes. Providing diabetes education and enhancing social support may also be important, as the demands/frustrations of living with diabetes and/or declining health may have significant psychological consequences.