Poster Presentation Australian Diabetes Society and the Australian Diabetes Educators Association Annual Scientific Meeting 2014
A multidisciplinary service for diabetes optimisation: a retrospective audit (#355)
Suboptimal glycaemic control is associated with diabetes complications. The Diabetic Support Service (DSS), a short-term, intensive, multidisciplinary clinic at Monash Health, Clayton was established to allow timely management for unstable patients with diabetes. Endocrinologists, diabetic educators and dieticians work together to support self-management, improve glycaemic control, manage and prevent complications. Referrals are accepted from GPs as well as other hospital departments, with a limit of 2-3 visits per referral episode. Patients are discharged back to their local GP with an ongoing management plan. More complex patients are referred to the chronic diabetes outpatient clinic for ongoing review. This retrospective audit assesses the efficacy of this intensive, multidisciplinary DSS in optimising diabetes management in an outpatient setting.
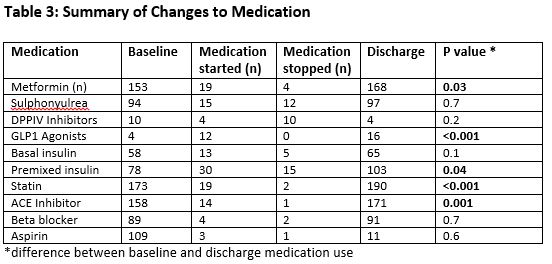
Medical records of patients attending the service over an 8 month period (January-September 2012) were retrospectively audited and clinical and laboratory parameters captured at baseline and discharge from the service. Medication use, including cardio-protective agents was also captured.
The files of 305 patients (mean age 57.5 ±16.6years, 57% male) were reviewed. The majority of patients had Type 2 diabetes (N=252, 82.6%), 32 (10.5%) had T1DM. Mean duration of diabetes was 10.6±9.8 years. Clinical characteristics are summarised in Table 1. Patients attended an average of 2.5 ±1.5 clinic visits. Significant reductions were achieved in HbA1c (mean difference 1.4 ±2.3%), blood pressure and total cholesterol level (Table 2) through intensification of glycaemic management and addition of antihypertensive and lipid lowering therapies, respectively (Table 3).
Diabetes is expected to become the highest contributor to disease burden in Australia by 20171. The impact of the growing diabetes epidemic on healthcare resources will be unsustainable without significant efficiency gains in service provision. Our data suggest that this novel model of service delivery which provides short term, intensive multidisciplinary and specialist management supporting primary care and patient self-management, is an effective way to improve diabetes control and cardiovascular risk in diabetic subjects at high risk of cardiovascular disease.
- Zimmet, P, Colagiuri, S, Gunton, J, Aylen, T, & Johnson, G 2013, A National Diabetes Strategy and Action Plan, Diabetes Australia, viewed 20 April 2014,