Poster Presentation Australian Diabetes Society and the Australian Diabetes Educators Association Annual Scientific Meeting 2014
Clinical outcomes of diabetic foot ulceration over two years since the inception of a High Risk Foot Service in a tertiary South-Western Sydney hospital. (#363)
Abstract
Background: The ADS recommends national data collection on the incidence and outcomes of diabetes-related foot complications(1). The NSW ACI Standards for High Risk Foot Services (HRFS) recommend collection of key performance indicators to assess safety, efficacy and to assist improvement of the clinical service(2).
Aim: To evaluate clinical outcomes of diabetic foot ulceration (DFU) managed by our HRFS.
Methods: Retrospective analysis of prospectively collected data (Oct 2011-May 2014) on patients with DFU and predominately type 2 diabetes. We analysed time to presentation to HRFS, time to and proportion of DFUs healed, hospitalisation, re-ulceration and amputation rates.
Results: There were 135 DFUs from 98 patients (mean age 66.2±13.8 years). Mean diabetes duration was 16.7±10.4 years and mean HbA1c 8.7±2.4%. 54% patients had previous DFUs (mean 1.74±1.0). Mean time DFU onset to HRFS assessment was 12.0±10.7 weeks. Wound severity at presentation (Texan Grading System)(3): 59.2% DFU were infected, 7.4% were ischaemic and 20% were infected and ischaemic (Table 1). 65.9% of all DFUs were superficial and 24.4% penetrated to bone.
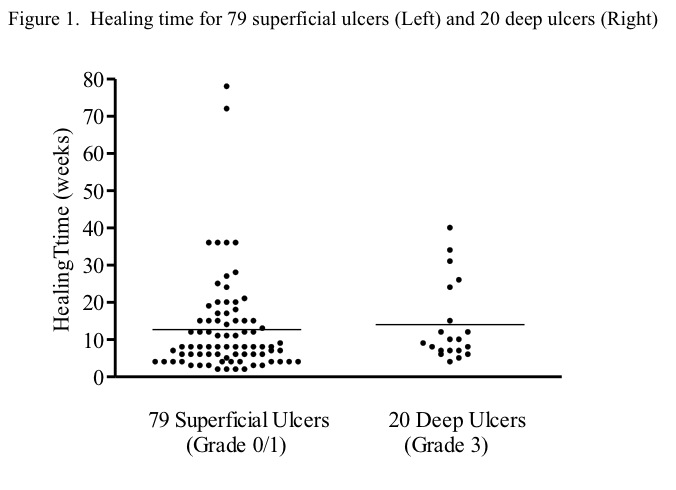
Healing rate was 90% (106/118, excluding 5 deceased and 12 lost to follow-up) with median time to healing 8 weeks. Healing time was longer for more severe wounds (14.0±2.4 weeks for Grade 3 ulcers versus 11.1± 1.0 weeks for superficial ulcers) but did not reach statistical significance (with exclusion of 2 skewed data points) (Figure 1). Hospitalisation for DFU was 21.5% (5 DFU requiring ≥2 admissions for IV antibiotics ± surgical debridement), re-ulceration rate 25.2% with median time to re-ulceration 24 weeks and amputation rate 8.9%.
Conclusion: Our HRFS has been able to achieve a high DFU healing rate with a relatively low amputation rate in a cohort of severe DFUs. Audit and reporting of key performance indicators from individual HRFS sites may assist with national data collection and improve service provision.
- Bergin SM, Alford JB, Allard BP, Gurr JM, Holland EL, Horsley MW, Kamp MC, Lazzarini PA, Nube VL, Sinha AK, Warnock JT and Wraight PR. A limb lost every 3 hours: can Australia reduce lower limb amputations in people with diabetes? Med J Aust 2012; 197 (4): 197-8.
- The Agency for Clinical Innovation (ACI) Endocrine Network: Diabetic Foot work group. The Standards for High Risk Foot Services (HRFS) in NSW. 2013 August. www.aci.health.nsw.gov.au.
- Armstrong DG, Lavery LA and Harkless LB. Validation of a diabetic wound classification system: the contribution of depth, infection, and ischemia to risk of amputation. Diabetes Care 1998; 21 (5): 855-9.