Oral Presentation Australian Diabetes Society and the Australian Diabetes Educators Association Annual Scientific Meeting 2014
Intensification from basal insulin in type 2 diabetes? Retrospective audit of clinical practice from four Australian centres (#196)
This retrospective audit of patients with type 2 diabetes mellitus (T2DM) in four Australian hospital clinics investigated treatment pathways after initiation of basal insulin. Included patients had been initiated on basal insulin and had a subsequent treatment intensification/change during the analysis period (Sept 2007–Mar 2012). Patients were classified into one of three intensification groups for analysis (Table).
Prior to basal insulin initiation, mean T2DM duration was 11 years. Between starting basal insulin and treatment intensification, 42/183 (22.9%) patients achieved the HbA1c target of <7%.
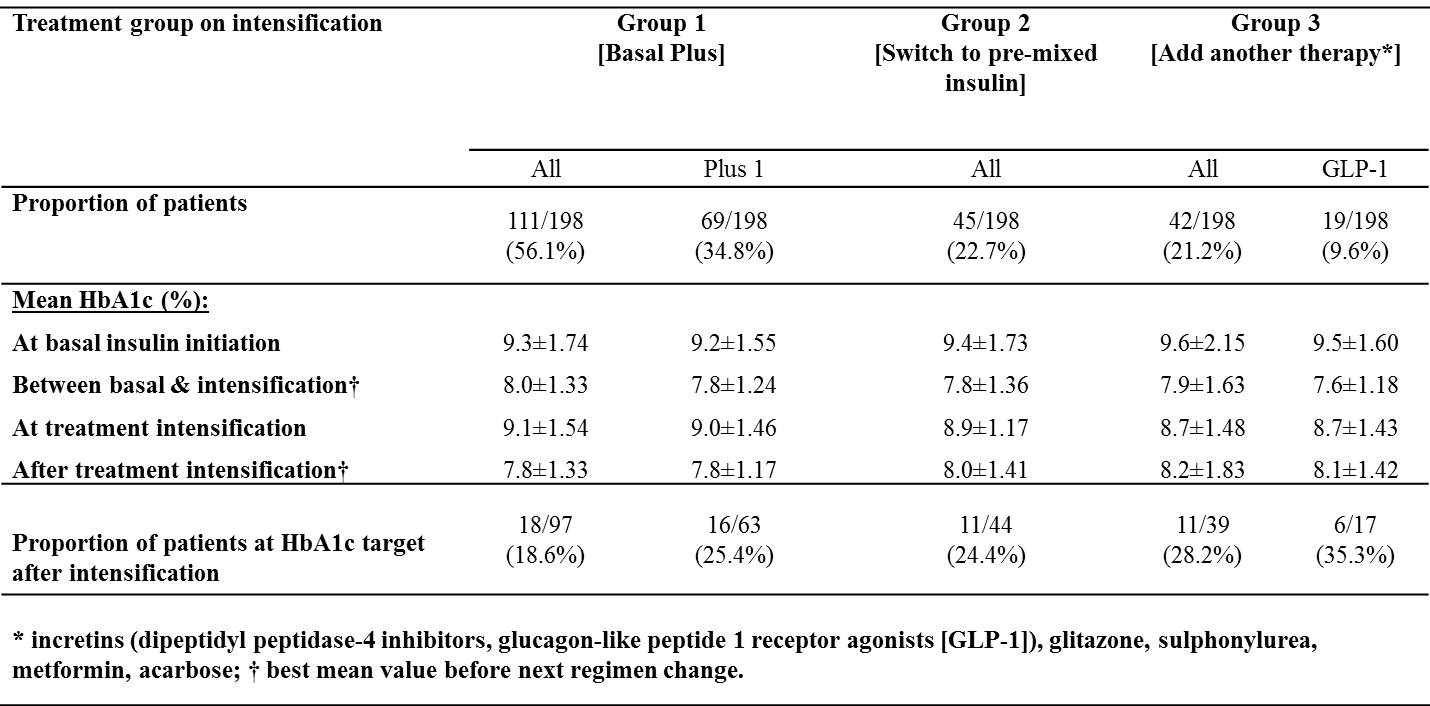
In this cohort, initiation of basal insulin provided temporary improvement in glycaemic control followed by subsequent deterioration. After treatment intensification 40/180 (22.2%) patients achieved the HbA1c target of <7%. Patients in the insulin groups gained weight (rapid acting insulin, 1.9±7.4Kg; premixed insulin 2.3±4.8Kg); those in Group 3 lost weight (-0.9± 13.54Kg). Hypoglycaemic episodes were uncommon irrespective of group.
To accommodate the progressive nature of T2DM; individualised management strategies should focus on when to initiate insulin, how to adjust and optimise doses over time and, when required, the introduction of intensification regimens.
Funding: This study and editorial support for the abstract were funded by Sanofi Australia Pty Ltd.