Oral Presentation Australian Diabetes Society and the Australian Diabetes Educators Association Annual Scientific Meeting 2014
Impact of Islet Cell Transplantation (ICT) on long-term diabetes complications two years post transplant (#191)
Aim
To evaluate the effect of ICT on progression of long-term complications, as compared with controls with recurrent hypoglycemia.
Method
18 subjects with recurrent hypoglycemia, 9 receiving ICT, were followed prospectively with baseline HbA1c, Hyposcore, mean glucose, SD, and percent time hypoglycemic and hyperglycemic from CGM. Complication screening was performed baseline and 2 years following medical treatment or ICT. Peripheral neuropathy was evaluated using thresholds for hot, cold and vibration; retinopathy was graded by retinal photography or external ophthalmologist; nephopathy by microalbumin excretion; autonomic dysfunction with pupillary response time1.
Results
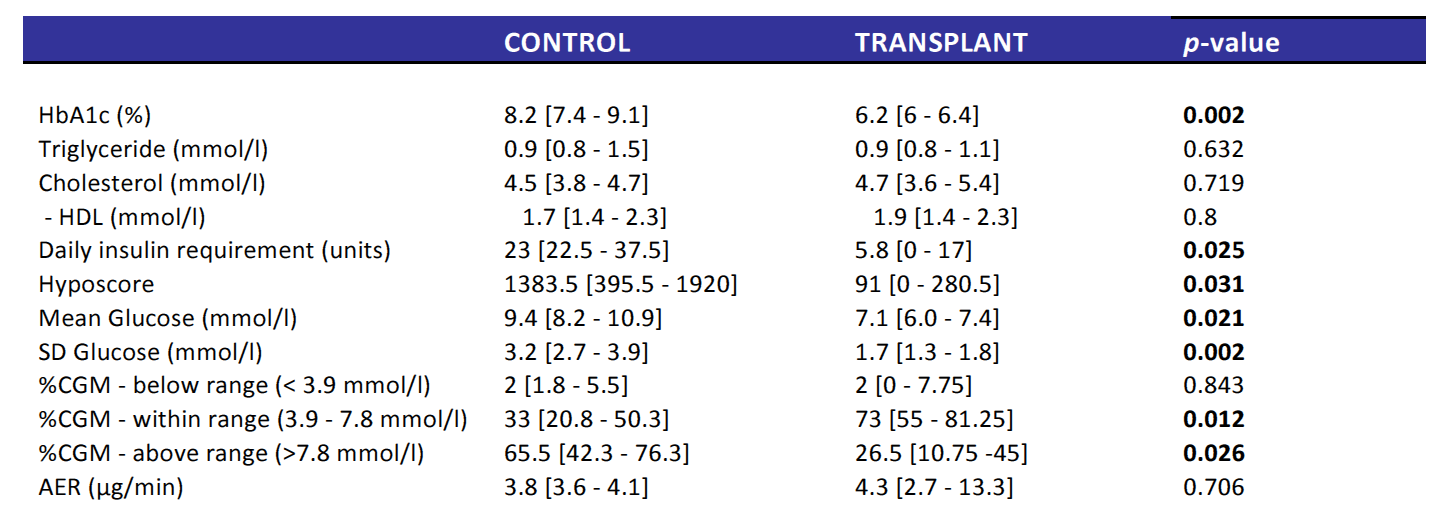
Clinical characteristics of control and ICT groups were similar at baseline. Two years post transplant (Table 1), there were significant between group differences in HbA1c, total daily insulin, Hyposcore, mean CGM glucose and SD glucose and percent time hyperglycemia. At 2 years peripheral neuropathy showed less progression in ICT than group (0% vs 33%, chi2=0.13). Using GEE, differences were predicted by Hyposcore (p=0.006), HbA1c (p=0.04), mean glucose (p=0.007), total daily insulin (p=0.01) and percent time hyperglycemic (p=0.02). Differences in pupillary response time were predicted by mean glucose (P=0.005) and percent time hyperglycemic (p=0.04) at 2 years. There were no significant differences at 2 years in retinopathy progression or microalbumin excretion but microalbumin excretion at 2 years was predicted by HbA1c (p=0.002), mean glucose (p=0.01) and baseline microalbumin excretion (p=0.02).
Conclusion
Improved glucose control and reduced hypoglycemia is achieved after ICT. Peripheral neuropathy progression was predicted by reduced hypoglycemia and improved glycemic control, post ICT and improvements in autonomic nerve function were predicted by improvements in glycemic control only.
- 1. Ferrari GL, et al. Using dynamic pupillometry as a simple screening tool to detect autonomic neuropathy in patients with diabetes: a pilot study. Biomed Eng Online. 2010 Jun 17;9:26.